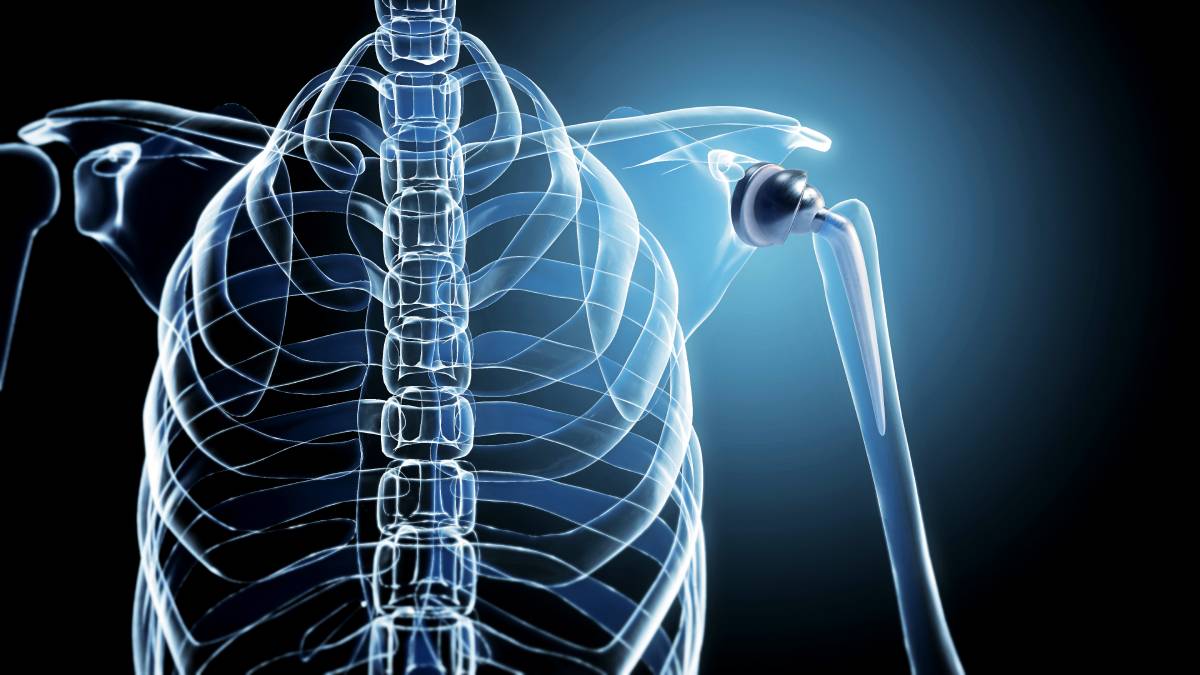
Total shoulder arthroplasty (TSA) is a surgical procedure that aims to provide relief and improved function for patients with severe shoulder pathologies, such as osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis (1). To ensure patient comfort and improve postoperative recovery, effective regional anesthesia techniques are essential during total shoulder replacement surgery. These techniques not only provide pain relief, but also reduce the need for systemic opioids and their associated side effects.
The shoulder is innervated primarily by the brachial plexus, a complex network of nerves that arise from the cervical and upper thoracic spinal nerves (C5-T1). The brachial plexus branches into several key nerves that are targets in TSA, including the suprascapular, axillary, and lateral pectoral nerves (1). Effective anesthesia for total shoulder replacement surgery involves targeting these nerves to ensure both pain control and muscle relaxation.
There are several nerve block techniques used in TSA, each targeting different nerves of the brachial plexus to optimize pain control. One of the primary blocks used is the interscalene brachial plexus block, which effectively numbs the nerves responsible for transmitting most shoulder pain. The interscalene block provides excellent analgesia but carries risks such as diaphragm paralysis due to phrenic nerve involvement, making appropriate patient selection critical (2). Another technique, the suprascapular nerve block, specifically targets the suprascapular nerve, which innervates approximately 70% of the shoulder joint. This block can be used alone or in conjunction with the interscalene block to improve pain control, which is especially beneficial in patients who are at significant risk for diaphragmatic paralysis. The axillary nerve block is another technique that is often used in combination with the aforementioned blocks to provide comprehensive coverage of the sensory nerves of the shoulder (2). This block is typically performed under ultrasound guidance to increase accuracy and reduce complications.
Advances in ultrasound technology have significantly improved the safety and efficacy of these nerve blocks by allowing anesthesiologists to visualize the nerve and surrounding tissue during the injection of anesthetic agents. The use of ultrasound has been shown to reduce the incidence of complications and improve the quality of the nerve block.
When selecting anesthetic agents, a variety of medications can be used for regional anesthesia for total shoulder replacement surgery. Bupivacaine and ropivacaine are commonly used local anesthetics due to their long duration of action, which is beneficial for postoperative pain management. These agents can be administered alone or in combination with adjuvants such as epinephrine, which prolongs the duration of the block and reduces systemic absorption, thereby minimizing toxicity. Recently, the use of liposomal bupivacaine, an extended-release formulation, has gained popularity (1). This agent provides prolonged postoperative analgesia, which can significantly improve patient comfort and reduce the need for additional opioid analgesia. In addition, adjuvants such as dexmedetomidine or dexamethasone are increasingly being used to prolong the effects of nerve blocks (3). These adjuvants, when added to traditional local anesthetics, have been shown to prolong the duration of analgesia without significant additional side effects.
The anesthesia approach for total shoulder replacement surgery should be individualized based on the patient’s specific medical condition, surgical procedure, and potential risk factors for complications. The integration of ultrasound-guided nerve blocks and the strategic use of long-acting local anesthetics and adjuvants can significantly improve the quality of postoperative pain management, thereby enhancing recovery and patient satisfaction in total shoulder arthroplasty.
References
- Fredrickson MJ, Krishnan S, Chen CY. Postoperative analgesia for shoulder surgery: a critical appraisal and review of current techniques. Anaesthesia. 2010;65(6):608-624. doi:10.1111/j.1365-2044.2009.06231.x
- Bishop JY, Sprague M, Gelber J, et al. Interscalene regional anesthesia for shoulder surgery. J Bone Joint Surg Am. 2005;87(5):974-979. doi:10.2106/JBJS.D.02003
- Vorobeichik L, Brull R, Abdallah FW. Evidence basis for using perineural dexmedetomidine to enhance the quality of brachial plexus nerve blocks: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2017;118(2):167-181. doi:10.1093/bja/aew411