In fast-paced medical environments, quick and accurate diagnostic information can be critical for guiding treatment. Point-of-care testing (POCT) is a growing concept in healthcare, especially in the context of anesthesia and surgery, that emphasizes real-time diagnostic results at the patient’s bedside.
POCT involves performing diagnostic tests at the “point of care” rather than sending samples to a centralized laboratory. This approach offers several advantages, including rapid turnaround time, enhanced workflow efficiency, and improved patient outcomes. By providing timely insights into a patient’s condition, POCT enables clinicians to make informed decisions promptly and gather more information for time-sensitive decisions 1.
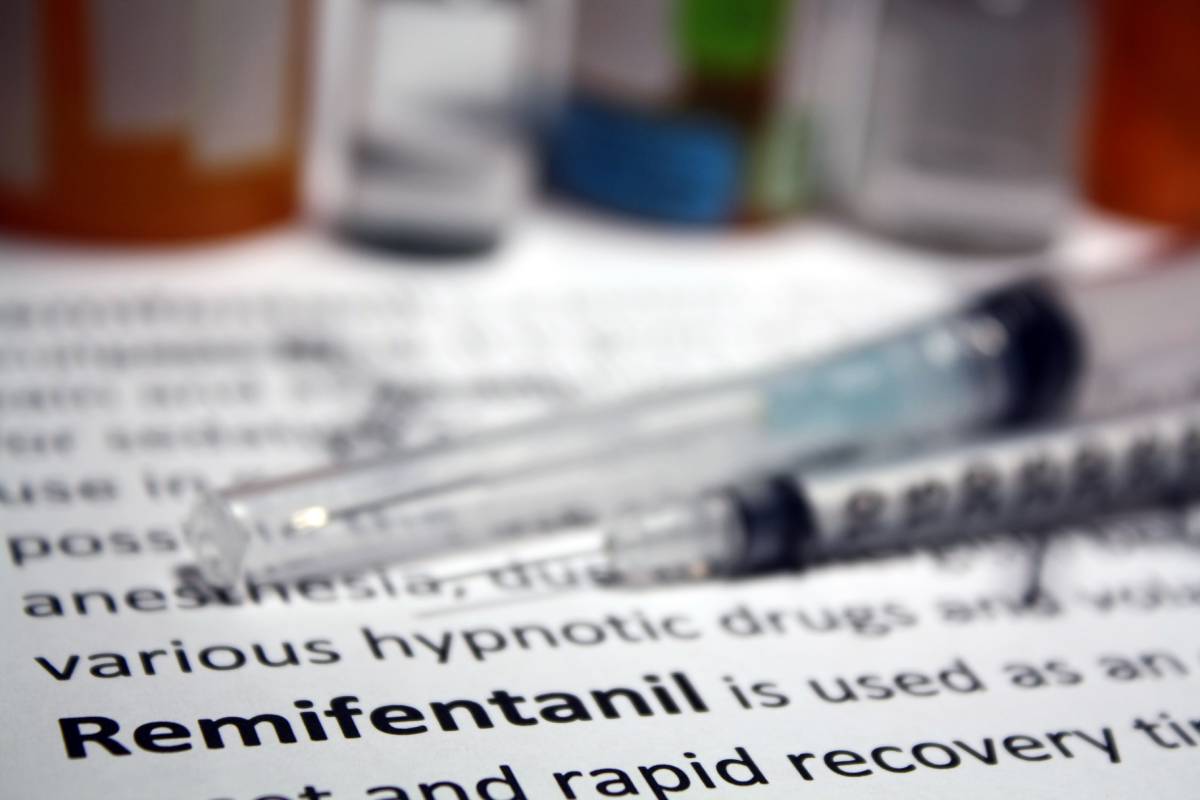
In the context of the operating room (OR), where speed and efficiency are particularly important, point-of-care testing has revolutionized the way surgical teams manage patient care. One of the most common applications of POCT in the OR is the measurement of blood gases and electrolytes. Monitoring arterial blood gas levels during surgery is crucial for assessing respiratory function, acid-base balance, and oxygenation status in critically ill patients. With POCT devices, doctors can obtain arterial blood gas results within minutes, allowing for prompt adjustments in ventilation and oxygen therapy to optimize patient outcomes 2.
Moreover, POCT plays a vital role in monitoring coagulation parameters during surgical procedures, especially in patients receiving anticoagulant therapy or undergoing major surgeries. Devices such as point-of-care coagulation analyzers enable rapid testing of clotting function, allowing surgeons to make timely decisions regarding blood transfusions, hemostatic interventions, and the management of bleeding complications 2.
Another area where point-of-care testing is making a significant impact in the OR is in the detection of infectious diseases. Rapid diagnostic tests for pathogens such as methicillin-resistant Staphylococcus aureus (MRSA) and Clostridioides difficile (C. diff) enable early identification of healthcare-associated infections to guide appropriate antimicrobial therapy and infection control measures. By identifying infectious agents quickly, POCT helps reduce the risk of postoperative complications and hospital-acquired infections, ultimately improving patient safety and outcomes 1.
Furthermore, POCT facilitates the monitoring of glucose levels in diabetic patients undergoing surgery, ensuring tight glycemic control and minimizing the risk of perioperative complications such as hyperglycemia and hypoglycemia. Portable glucose meters allow surgical teams to perform frequent blood glucose measurements intraoperatively, guiding insulin administration and fluid management strategies to maintain optimal metabolic balance 1,3.
POCT offers clinical and clear logistical advantages. By eliminating the need to transport samples to a central laboratory and wait for results, it reduces turnaround times and streamlines the decision-making process during surgery. This not only enhances workflow efficiency but also conserves valuable resources and reduces healthcare costs associated with traditional laboratory testing 4.
However, point-of-care testing in the OR also has some disadvantages. Quality control, operator training, and compliance with regulatory standards are essential to ensuring the accuracy and reliability of results. Moreover, interoperability and integration with electronic medical records systems are crucial for data management and documentation in the perioperative setting 4.
Overall, point-of-care testing is advancing healthcare delivery by providing rapid and reliable diagnostic information that empowers surgical teams to make informed decisions and optimize patient care. As technology continues to evolve, the integration of POCT into routine practice is poised to further enhance patient safety, outcomes, and overall experience.
References
- Point-of-Care Testing – StatPearls – NCBI Bookshelf. Available at: https://www.ncbi.nlm.nih.gov/books/NBK592387/. (Accessed: 17th March 2024)
- Point-of-Care Testing – Testing.com. Available at: https://www.testing.com/articles/point-of-care-testing/. (Accessed: 17th March 2024)
- Point of Care Testing | Sight Diagnostics. Available at: https://sightdx.com/en/knowledge-center/point-of-care-testing. (Accessed: 17th March 2024)
- Point of Care Testing (POCT). Available at: https://www.leedsth.nhs.uk/a-z-of-services/pathology/poct/. (Accessed: 17th March 2024)